Using artificial intelligence, WashU Medicine researchers from neurosurgery and computer science have identified 3 subtypes of Chiari type-1 malformations that could improve medical decision making
By: Mark Reynolds
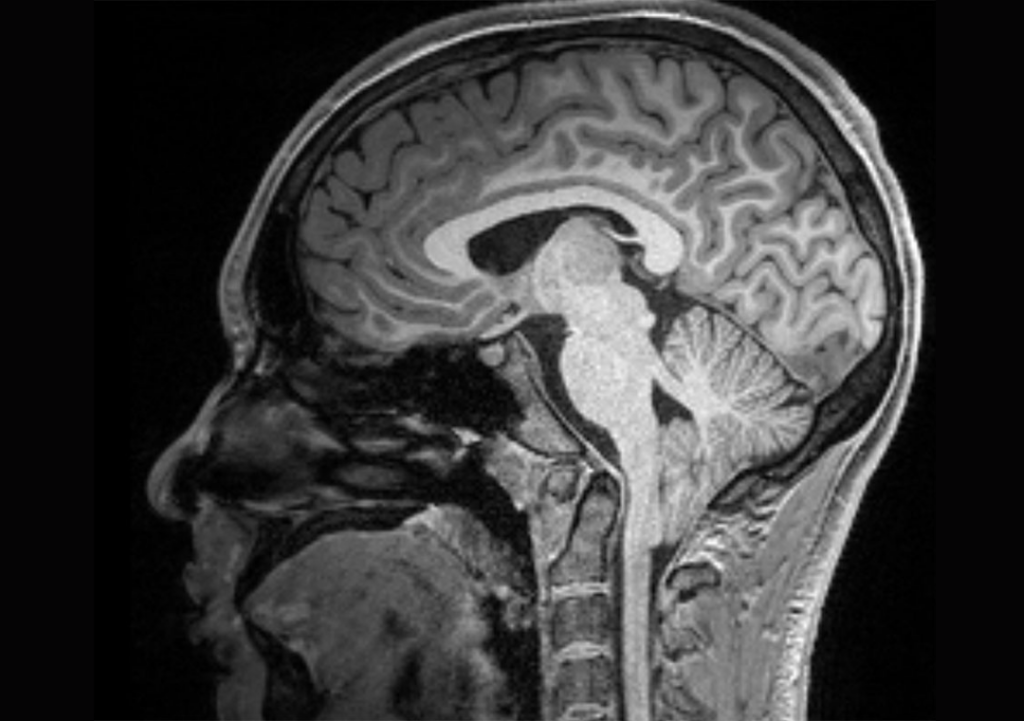
Roughly 4% of the population is affected by a congenital brain malformation that has eluded researchers’ efforts to find causes and treatments. For the condition, Chiari type-1 malformation, the diagnosis is straightforward: the lower part of the brain, known as the cerebellum, protrudes at least five millimeters through the gap in the skull that connects to the spinal cord.
There’s no one known cause for Chiari type-1, and the symptoms it can cause are unpredictable. The most common problems include chronic headaches, difficulty swallowing and decreased muscle strength, as well as syringomyelia, a condition that occurs when a cyst forms in the spinal cord. Sometimes these symptoms occur in combination, or singly. In most cases, people can live their whole lives with no ill effects. The breadth of Chiari type-1 presentations has made it difficult for physicians to develop a consistent treatment protocol for their patients.
A study by Washington University in St. Louis researchers has begun to fill that gap. A collaboration among neurosurgeons and computer scientists has defined three sub-types of Chiari type-1 with distinct characteristics that physicians can use to plan treatment options for their patients.
The results are available in the Journal of Neurosurgery.
More and better information was needed to refine Chiari type-1 diagnoses so doctors could reliably determine which cases call for which clinical interventions, if any. For instance, a surgical operation can widen the opening at the base of the skull to reduce pressure on the brain and relieve certain symptoms in some Chiari type-1 patients.

“Chiari represents a substantial proportion of all the patients that pediatric neurosurgeons see – it’s probably in the top three leading causes of surgeries,” said Sean Gupta, MD, a neurosurgery resident at WashU Medicine and a co-lead author of the study. He explained that not every type of patient responds to or needs the procedure. It is particularly necessary in patients who present with both syringomyelia and headaches, though some patients continue to experience effects despite surgery. Other cases may be managed with pain medications or monitored. Most cases remain undetected to patients and their doctors alike.
“In some population studies, looking at a random selection of people who had MRIs but no diagnosis, when we specifically look for Chiari malformations you find something like up to 4% of the population has it, but it doesn’t necessarily cause them any problems,” Gupta said.
For the cases that are affecting the health and quality of life of patients, doctors only had incomplete information on how and when to best treat a spectrum of symptoms that did not always respond to interventions in the same way.
There was no shortage of available data to search for patterns in malformations and symptoms to identify subtypes for which treatment protocols could be devised. WashU Medicine is the lead institution in the Park-Reeves Syringomyelia Research Consortium, with information from more than 1,200 patients with Chiari type-1 to comb for correlations. There are, in fact, hundreds of variables for each patient — ranging from clinical data and brain imaging to health insurance status. For the model, a subset of these variables was carefully selected using a combination of data-driven methods and clinician input, gathered through a survey of expert pediatric neurosurgeons nationwide.
“It’s what we call a very high-dimensional problem, in that there are many variables that have to be considered,” said Chenyang Lu, PhD, a co-senior author of the study and the Fullgraf Professor of Computer Science & Engineering in the McKelvey School of Engineering and founding director of the AI for Health Institute at WashU. Co-senior author David Limbrick, MD, PhD, now the James W. and Frances G. McGlothlin chair of the Department of Neurosurgery at Virginia Commonwealth University School of Medicine, approached Lu because the artificial intelligence tools like those with which he works are extremely good at sifting through large data sets to identify patterns and correlations within the many variables associated with Chiari type-1 cases. These patterns could then serve as indicators to physicians seeking the best treatment options for their patients.
Ziqi Xu, a PhD student in the Lu lab at WashU and co-lead author, developed the AI algorithm to sort through which of the 500-plus variables in the dataset clustered together. Three distinct subtypes of Chiari type-1 emerged.
Cluster 1 patients were more likely to be female, tended to be diagnosed slightly later in childhood and presented with chronic headaches and few other health issues. Cluster 2 patients were younger and had fewer headaches but a wider range of other issues such as muscle control and swallowing difficulties. The third cluster usually presented with spinal deformities, which may require the standard decompression procedure and possible further spine surgeries.
“This should help in the effort to develop guidelines that will decide which patients need to get surgery, and what type of surgery, or what other therapy may need to happen,” Gupta said. “We need to have some sort of evidence-based consensus opinion on how a clinician treats or manages these patients. Until now we have been working from very imperfect data.”
Xu, who is already working to further refine and develop this model, said she believes that the collaboration between clinicians and computer scientists in this study has the potential to be transformative across the field of medicine.
“We are in a golden age,” Xu said. “With the growing power of computational tools and the vast data in electronic health records, AI can serve as a catalyst for generating novel insights for clinicians, enabling us to work together toward impactful discoveries and better patient care.”
Gupta VP, Xu Z, Greenberg, JK, Strahle JM, Haller G, Meehan T, Roberts A, Limbrick Jr DD, Lu C. Using artificial intelligence to identify three presenting phenotypes of Chiari type-1 malformation and syringomyelia. Neurosurgery. Nov. 18, 2024 DOI: 10.1227/neu.0000000000003249
Neurosurgery is the official publication of the Congress of Neurological Surgeons, published in the Lippincott portfolio by Wolters Kluwer.
This project received grant funding from the Neurosurgery Research and Education Foundation (NREF) 2023-24 NREF & AANS/CNS Section on Pediatric Neurological Surgery Research Fellowship Grant (VPG) and the NIH NINDS P01NS131131-01 5758 Program Project Grant (DDL). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,900 faculty. Its National Institutes of Health (NIH) research funding portfolio is the second largest among U.S. medical schools and has grown 56% in the last seven years. Together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,900 faculty physicians practicing at 130 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.