Six months before COVID-19 hit, Chad Washington, MD, MS, was promoted to chair of Neurosurgery at University of Mississippi Medical Center, the only academic medical center in the state. Specializing in adult cranial neurosurgery and vascular neurosurgery, Dr. Washington credits his training at Washington University – and some key people – for profoundly influencing his career.

Washington graduated Phi Beta Kappa from Millsaps College, in Jackson, Mississippi and completed an MS in Biomedical Engineering at Vanderbilt University. He received his MD from the University of Mississippi Medical Center.
During his neurosurgical residency at Washington University in St. Louis, Washington obtained an MS in Population Health Sciences and completed an international fellowship at the National Neurosurgical Centre in Dublin, Ireland. Following residency, he completed a fellowship in endovascular neurosurgery, also at Washington University.
Q. What do you find most rewarding about being a neurosurgeon and your role as chair?
A. I enjoy the technical aspects of neurosurgery and the exactness of the surgeries. I enjoy our work in neuroanatomy, and how the brain interacts with the rest of the world through our bodies. I enjoy my role in helping patients to maximize that, as well as taking care of some of the most critically ill patients who are dealing with difficult diagnoses. Patient engagement is at a very personal level with neurosurgeons. The ability to help people and get them back into their lives, it is rewarding.

In terms of what I enjoy about being chair, our role at UMMC is unique within the state. We take care of patient populations – in terms of diagnoses and critical illness — that really nowhere else in the state you’re able to do. Being that sort of safety net of neurosurgical care within the state is very rewarding. It provides you with the ability to really make a difference on not just the individual patient level, but also on a wider, broader range across the state of Mississippi.
I’m proud of that, and I’m proud to serve with a group of people who really see the patients that we take care of as their family. I’m also proud to train the next generation of neurosurgeons coming through medical school and residency.
Q. Why did you choose to do your training at WashU?
A. Whether I was going to be a private practice neurosurgeon who came back to Mississippi, an academic neurosurgeon, or go into research, I wanted a program with a broad exposure to the complete spectrum of neurosurgery. WashU offered this, and it was a great program.
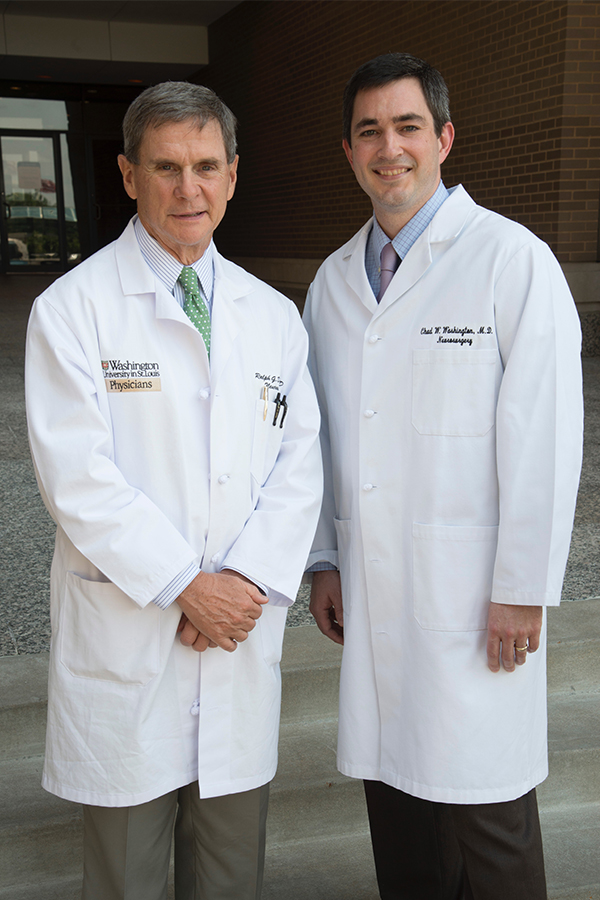
Washington University Neurosurgery’s former Chair Dr. Ralph Dacey and current Chair Dr. Gregory Zipfel are professionally two of the most influential people in my life as far as my career path, and I greatly appreciate what they have done for me, have given and continue to give. I sincerely appreciate the time and effort that they and the attendings at Washington University spent on me in my residency.
On this side of things, I understand now more clearly than ever that it really does take a person who is invested in the residents. It’s evident to me that they are invested in their residents, invested in their training and really do want us to succeed.
There’s faculty there who I trained with, and there’s faculty there that trained me, and it holds a very special place in my heart. It was a great experience.
Q. What stands out to you about WashU’s residency program?
A. The high level of expectations placed on the residents. We were not just a workforce within the department. We were expected to be totally engaged with patient care, and with that came a lot of responsibility.
As you go through the program you gain more autonomy within the operating room. That culminates in the chief year where there’s a very high level expected of you to operate essentially almost as an independent neurosurgeon, with appropriate oversight. I think that final year of very intense operative experience is critical in your training.

With WashU, there is also the Ireland experience. That is phenomenal opportunity for the residents at WashU. The Irish medical system is set up differently than ours. You go over as a senior resident, and they provide you with an opportunity to operate under a level of independence that you don’t get here in the states very often.
This exposure to a different way of managing surgery teaches you a perspective of neurosurgery that is unique. You have the responsibility of making difficult decisions about bringing patients from one hospital to another. Making those decisions, it’s very beneficial in our training. It’s a phenomenal experience amongst the residents and their faculty and affords the opportunity to travel across Ireland and Europe. That’s exposure that I don’t think many people get.

Q. What experience has taught you the most?
A. Being chair of a department is probably the most rapid learning experience I’ve had. I became chair in July, and six months later, COVID hit. We were shutting down operating rooms. Faculty residents, and staff in the department were all unsure of what the future held. My goal was to try and be a steading force that they can look up to and help reassure them that things are going be okay.
Q. How else have you and your team been affected by COVID-19?
A. Seeing patients without COVID who have been affected by having their surgeries delayed, or their overall care delayed, is hard. On a personal level, there is that disconnection from having patients in these isolation rooms, who are not able to be next to their loved ones. Then having to see the family struggle with not being able to be next to their families in these critical times.
When COVID hit, this new dynamic between patients, physicians and families developed. Our palliative care team took on a different role to be this patient experience engagement team, where they were a critical group helping with the communication between those parties. I relied a lot on people within the hospital and other partners to help with that. Individually as a department, we made a concerted effort to have someone from our team communicate with families, on a regular, regimented schedule.
Q. Do you have any advice for future residents or anybody looking to practice medicine?

A. I would say for medical students, and people going into medicine who are considering neurosurgery, understand that training is hard. And it needs to be hard, because we’re dealing with very complex diagnoses; we’re having to do very complex procedures. The patients deserve to know that their neurosurgeon is the best neurosurgeon they can possibly be. To train someone effectively, in a set amount of time, it takes a very intense and regimented training program.
While sometimes it is tough, the rewards are good. In terms of the residents transitioning from residency to their careers, be the type of person that people are rooting for. Be someone that people see as a problem solver, not the one that’s always complaining. Complain when necessary, and when it’s at the patient’s best interest, but do it at the right time. Those are some of the things that I see people struggle with the most.
